How to Treat a Herniated Lumbar Disc At Home

A herniated lumbar disc is an unfortunate—but not uncommon—injury that can occur when you least expect it.
Case Study: Michael’s Unexpected Setback
Michael, a middle-aged financial advisor, never imagined that such a simple action could so drastically alter his daily life. One ordinary afternoon, he stooped to lift a light box—a routine task he had performed countless times previously. This time, however, he felt a sharp twinge shoot through his lower back. And in an instant, he had suffered a herniated lumbar disc.
The days that followed were frustrating as Michael worked to manage his pain. He grappled with the irony of what felt like a disproportionate injury. How could lifting a feather-light load lead to such a significant setback? He resolved to reevaluate his approach to lifting objects, heavy or not, as he shifted his focus to recovery.
Along the way, Michael discovered several strategies for treating his injury. I’ll outline some of these in this article, as well as answer other questions you may have about a herniated lumbar disc.
What is a Herniated Disc?
A herniated disc—sometimes called a “slipped” or “ruptured” disc—is a condition that affects the intervertebral discs in the spine. Intervertebral discs act as cushions or shock absorbers between the vertebrae (bones) of the spine, allowing flexibility and movement.
When a disc herniates, its soft, gel-like center (or nucleus pulposus) protrudes through a tear or rupture in its tough outer layer (or annulus fibrosus). The displaced material can put pressure on nearby nerves, leading to symptoms such as pain, numbness or weakness in the affected area.
Herniated discs commonly occur in the lower back (lumbar spine) but can also affect the neck (cervical spine) or, less frequently, the upper back (thoracic spine).
What Causes a Herniated Disc?
Several factors can contribute to the development of a herniated disc, including the following:
- Age: Discs naturally degenerate over time, making them more susceptible to herniation, especially in individuals over 30.
- Fitness level: General strength and condition of abdominal muscles can often dictate how easy it is to herniate a disc.
- Pregnancy: Women who have undergone pregnancies may have weakened abdominals from stretching in the abdomen. C-sections can contribute even more to abdominal muscle weakness, since some of the affected muscles are surgically cut during the procedure.
- Repetitive Strain: Activities that involve repetitive or heavy lifting or bending, twisting or straining the spine can contribute to disc herniation.
- Trauma: Injuries to the spine—such as a sudden impact, fall or motor vehicle collision—can cause discs to herniate.

Herniated lumbar discs often occur from bending forward, as in Michael’s example of picking up something light. Symptoms can vary depending on the location and severity of the herniation. Common symptoms of a herniated lumbar disc include localized pain in the low back or radiating pain. Tingling, numbness, and weakness can also occur shortly after the initial pain. Treatment options range from conservative measures—such as rest, medication, and physical therapy—to more invasive interventions such as injections or surgery, depending on the severity and persistence of symptoms.
If you suspect you have a herniated lumbar disc or are experiencing persistent back pain, seek medical attention for a proper diagnosis. It’s important that you promptly begin a treatment plan tailored to your specific situation.
Will a Herniated Disc Get Better Without Surgery?
In many cases, a herniated disc can improve on its own with conservative, non-surgical treatments. The body has a natural ability to heal; given time, the symptoms of a herniated disc may resolve.
However, it’s important to note that the timeframe for recovery can vary greatly among individuals. In rare cases, symptoms may persist beyond these conservative measures.

How to Treat a Herniated Lumbar Disc at Home
Treating a herniated disc at home involves a blend of self-care techniques. But before trying these techniques, it’s essential that you consult a healthcare professional for guidance, especially if your pain is severe or accompanied by other symptoms. Below are some general tips that may alleviate your discomfort.
Rest
For the first 24–48 hours, when the pain and limitation are most acute, try to take it easy. Avoid any activities that worsen the pain. If you have an upcoming golf or tennis date, it may be best to cancel, at least until your symptoms resolve. On the other hand, try not to remain immobile for extended periods. Find a balance between sitting and getting up every 45–60 minutes.
Limit bending over or twisting in the spine
As much as within reason, limit yourself from bending forward or twisting in your spine These movements can aggravate the pain, especially for the first 3–5 days after the injury.
Cold and Heat Therapy
Applying ice packs (for the first 48 hours) and then switching to heat (hot baths or heating pads) can help ease muscle spasms, reduce inflammation, and optimize the healing process.
Over-the-counter (OTC) Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen may alleviate pain and inflammation. Always follow dosage instructions and consult a medical professional if you take other medications or have allergies to certain NSAIDs.
Proper Posture
Maintaining good posture can alleviate pressure on the spine. Use ergonomic chairs with lumbar support, avoid slouching, and practice proper lifting techniques. When sitting or sleeping, strategically place pillows to support your lower back and help your body further relax.
Bracing
An over-the-counter back brace can provide passive support and ensure some relief, when worn properly. And if you feel silly wearing a brace, consider: your back has worked hard enough to get to this point; it deserves a little vacation.
Remember, your approach with these techniques will vary based on the severity and condition of your herniated disc. Always consult a healthcare professional for a proper diagnosis and personalized treatment plan. If you experience severe or worsening pain, numbness, or difficulty controlling bowel or bladder function, seek immediate medical attention.
3 Herniated Disc Exercises to Relieve Pain
For most individuals, the best thing you can do to minimize symptoms in the first 24–48 hours is to relax and reduce your activity. After the first two days, introduce some of the following movements to help lessen pain and prevent a recurrent herniated disc.
The common theme with these exercises is that they encourage a straight back position, otherwise known as an extension position.
- Standing lumbar extension
- While standing, place your hands on your lower back.
- Gently arch your back to look at the ceiling.
- Repeat 5–10 times, holding for 2–3 seconds each repetition.
- Limit the range of motion, such that no irritation occurs.
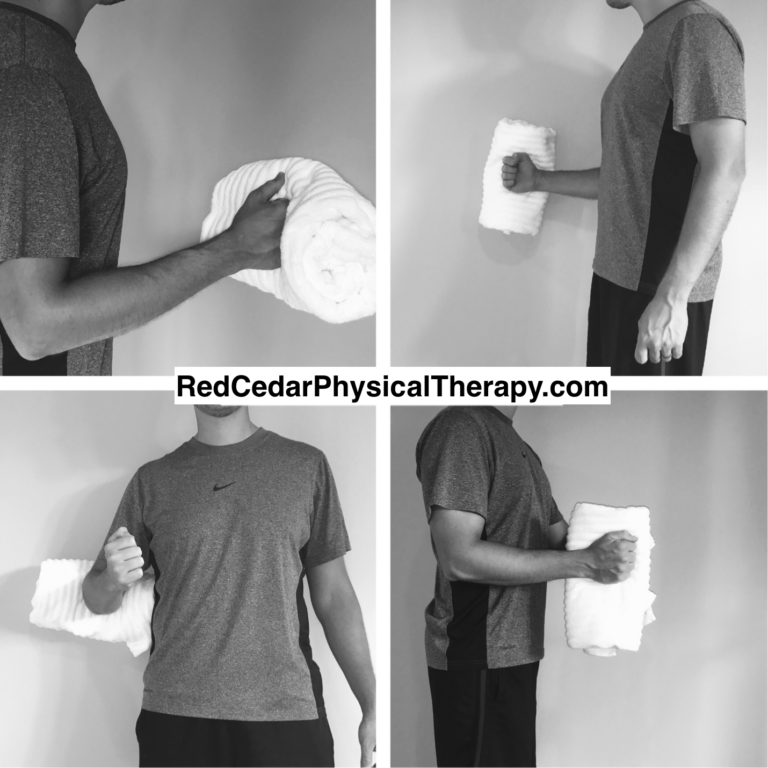
- Hip Hinge
- While standing, place your hands on the front of your hips, right below the belt.
- Keeping your back flat, lean forward by hinging at your hips, not bending your back.
- Repeat 5–10 times.
- Camel stretch
- Get on your hands and knees (on a couch or bed; getting on the floor may aggravate your symptoms).
- Allow your lower back to sink toward the floor by gently tightening the muscles in your upper back and drawing your shoulder blades together.
- Repeat 5–10 times.

What Are Some Signs I Should Go See a Doctor?
While some cases of a herniated disc can improve with conservative measures, certain signs and symptoms (also known as “red flags”) warrant prompt medical attention. If you experience any of the following red flags, you should seek medical help:
Worsening Pain
If the pain becomes increasingly severe or is not alleviated by rest and over-the-counter medications, consult a healthcare professional.
Pain at Rest or Night Pain
If you experience pain while at rest or during the night, it may indicate a more serious condition that requires medical attention.
Severe or Progressive Weakness
If you notice a sudden or progressive weakness in your legs or difficulty lifting your foot, it may indicate nerve compression. Medical evaluation is crucial.
Difficulty Walking or Coordination Issues
If you experience difficulties with balance, coordination, or walking, it may suggest nerve involvement requiring medical assessment.
Pain Radiating Down the Arm or Leg
Persistent, radiating pain, especially if accompanied by numbness or weakness, may indicate nerve compression and should be evaluated by a healthcare provider.
Unexplained Weight Loss
Unintentional weight loss combined with back pain may be a sign of an underlying issue that needs investigation.
Loss of Bowel or Bladder Control
This is a serious symptom that requires immediate medical attention. It could indicate cauda equina syndrome, a rare but severe condition resulting from significant compression of the spinal nerves.
Numbness in the Genital Area
Also known as “saddle anesthesia,” unexplained numbness or tingling in the genital region can be a sign of nerve compression and should be evaluated promptly.
Remember that each person can experience symptoms differently, and these red flags are not exhaustive. If you are uncertain about your symptoms or have concerns about your back pain, it is crucial that you consult a healthcare professional for a thorough evaluation and appropriate guidance. Early diagnosis and intervention can contribute to better outcomes in managing herniated disc-related symptoms.
Consider Seeing a Physical Therapist
If your herniated disc symptoms persist, physical therapy can provide a helpful form of conservative treatment. A physical therapist (PT) will evaluate and assess your body to see if there are any particularly stiff areas that need stretching or muscles that need strengthening. Based on their evaluation, your PT will provide stretching exercises appropriate for your herniated lumbar disc. If seeing a physical therapist in an outpatient clinic is not feasible, consider a concierge Physical Therapist, like the team at Red Cedar Physical Therapy.
It may be a good idea to see a PT if you have recurrent back pain issues. They can give you strategies for addressing the areas of weakness or stiffness that contribute to your chronic back pain. Your herniated disc may indicate that you’ve been performing some movements improperly, increasing your risk of re-injury.